What is Lambeth DataNet?
DataNet aims to support the health system in Lambeth by promoting research and intelligence to improve health and provide more equitable care within our community, through a locally driven, standardised, high quality data set.
Some prominent research using DataNet has featured in articles by the BBC (May 2023) and the London Evening Standard (March 2023).
Why is Lambeth DataNet unique and different to other national information collection schemes?
Lambeth DataNet is unique for three reasons:
- Lambeth DataNet collects local data, which is anonymised at the source so no identifiers leave the general practice and no identifiers can be traced back to patients
- Lambeth DataNet information can be associated with individual GP practices so results can be used to improve services locally
- Data will never be shared for commercial purposes
What if I don’t want to share my information with DataNet?
DataNet treats its responsibility for ensuring patient confidentiality with the utmost seriousness and has strict rules and governance processes in place to ensure that patients’ personal information remains confidential. We previously commissioned Healthwatch Lambeth to undertake an independent project to establish and evaluate a method of promoting transparency in how patient data is being used in Lambeth to improve services.
We hope to have information from all patients registered at GP practices in Lambeth. This will enable us to obtain information to reduce health inequalities and ensure a fair distribution of services to communities with the greatest health need. However, if you are not happy about sharing your information to improve services, you can opt out by letting your GP practice know. You can do this by writing to them, emailing them or going to the surgery.
Want to know more?
If you’re interested in Lambeth DataNet research findings, would like to propose a research question, or would like more information on how Lambeth DataNet has been used in commissioning or policy, please email us at PublicHealth@lambeth.gov.uk
Lambeth DataNet projects summary update: March 2023
Here are some of the key research outputs from DataNet over the past 12 months.
Primary Care Consultations
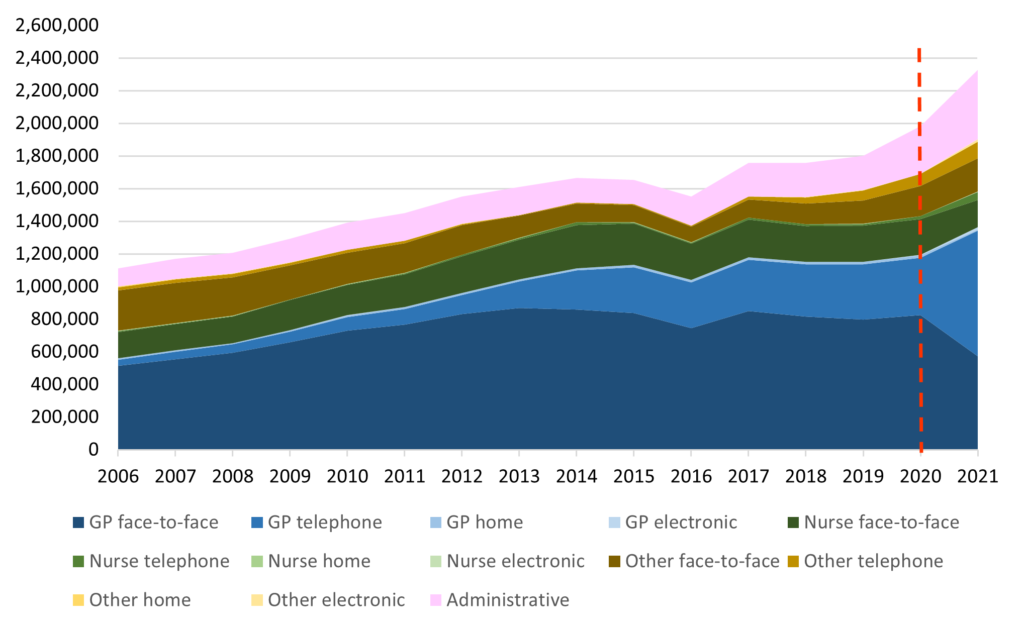
Primary care workload as measured by consultation rates per 1000 registered patients have increased progressively since 2005; consultation rates are now higher post-pandemic than before the first Lockdown.
Primary care consultations by mode of delivery and provider type, 2006-2021
Journey to multimorbidity
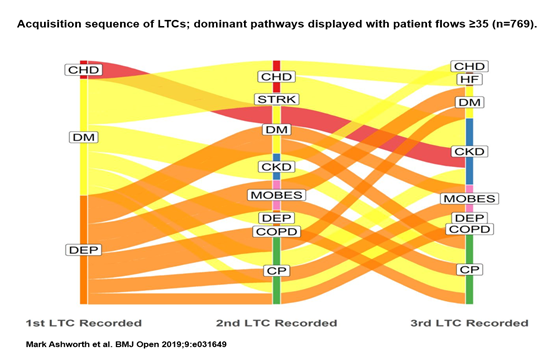
We have been studying the ‘starter conditions’ for patients who end up with 3 or more long term conditions. Here, depression and diabetes were the most common starter conditions for patients who went on to develop 3 or more long term conditions. The most common starter conditions differ according to social deprivation and ethnicity; more details using the same type of diagram are available here: https://bmjopen.bmj.com/content/9/12/e031649
Multimorbidity and depression
We have found that for patients with multimorbidity, any combination of long term conditions that includes depression results in double the number of primary care consultations: https://bjgp.org/content/71/702/e39
This shows the importance of addressing the mental health needs of patients with multimorbidity; also the possible role of other agencies such as IAPT (psychological therapy) services to reduce high demand on primary care services for patients with combined mental health and physical health multimorbidity.
Health inequalities: prevalence of long term conditions
Prevalence of ‘Top 12’ long term conditions in adults registered at GP practices in Lambeth; data for whole adult population:
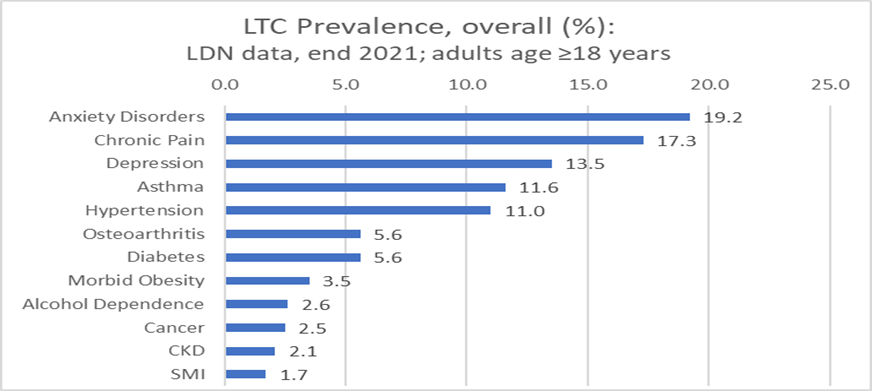
However, this pattern of conditions varies according to social deprivation, ethnicity and gender. For example, hypertension rates are 3 times higher in Black ethnicity women compared to White ethnicity women; chronic pain rates are twice as high in Black ethnicity women compared to White ethnicity women; diabetes, chronic pain and hypertension rates are more than 50% higher in deprived communities (comparing most and least deprived quintile of population).
Other studies
- Serious Mental Illness (SMI) in the Somali population and optimising treatment; Research lead: Peter Schofield (work in progress)
- Pre-conception health inequalities: large differences found in detection of physical and mental health conditions in women at preconception stage; which may account in part for higher mortality for Black and Asian women in the perinatal period; Research lead: Raquel Catalao; published in BMJ Open: http://dx.doi.org/10.1136/bmjopen-2021-059257
- Post-natal primary care: the diagnosis of hypertension and diabetes during pregnancy – and what happens to these conditions in the years after pregnancy; Research lead: Liza Bowen (work in progress)
- Dementia: evidence of poor DM control in patients with early or moderate dementia. Research lead: Usha Gungabissoon; published in JAMDA: https://doi.org/10.1016/j.jamda.2022.04.045
- Dementia: the recorded prevalence of dementia is likely to be an underestimate. Dementia in patients with frailty is often not recorded and these patients are often not referred to dementia services; Research lead: Mariam Molokhia; published in Age and Ageing: https://doi.org/10.1093/ageing/afab164
- Health Checks in primary care: uptake of cardiovascular health checks higher in Black Caribbean and Bangladeshi community; lower in ‘White Other’ communities (mostly Latin American/Eastern European). The value of Health Checks for tackling inequalities could be strengthened by better targeting; Research lead: Mariam Molokhia; published in Lancet eClinical Medicine: https://doi.org/10.1016/j.eclinm.2022.101471
Work presented at SAPC and Heart UK conferences 2021 & 2022
- Social determinants of diabetes, hypertension, stroke and CHD in Black ethnicity women: Deprivation and health-related behaviours made notable contributions to known inequalities in cardiovascular risks between Black African, Black Caribbean, and White ethnic groups; Research lead: Mariam Molokhia; published in Lancet Public Health: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02639-8/fulltext
- Familial hypercholesterolaemia (FH): Study of ethnic disparities in FH detection and management. Health disparities may exist due to cases being missed particularly in Chinese and Black African ethnic groups. Key finding: 20% of FH coded patients not taking lipid-lowering medications. Notably low rates of FH recording in non-English speakers; Research Leads: Mariam Molokhia, Tony Wierzbicki; funded by NHS South East Genomic Medicine Service Alliance (SE GMSA) and NHS Race & Health Observatory. https://www.england.nhs.uk/london/wp-content/uploads/sites/8/2019/08/3.1.1-Familial-Hypercholesterolaemia-a-Primary-Care-Perspective-Presentation-2019.pdf and https://www.kcl.ac.uk/news/new-study-seeks-to-improve-identification-of-inherited-high-cholesterol
- Undiagnosed CKD: almost half those with CKD are undiagnosed; half those with CKD (both diagnosed and undiagnosed) also have hypertension but often undiagnosed or undertreated; statins were prescribed to less than half those with CKD; Research lead: Mariam Molokhia; published in J Nephrol: https://doi.org/10.1007/s40620-021-01149-0. Also picked up by NIHR as a Key Evidence Message: https://evidence.nihr.ac.uk/alert/chronic-kidney-disease-is-often-undiagnosed-and-untreated/
- Fit Notes and mental health problems: Patients with either Chronic Pain or Depression had the highest rate of Fit Notes. Fit Notes were more likely to be issued to patients living in the most deprived communities; Asian and White ethnicity were associated with low use of Fit notes whereas Black ethnicity was associated with higher use of Fit Notes, likely the result of more Long Term Conditions that impair ability to work; Research lead: Sarah Dorrington; published in BMJ Open: https://oem.bmj.com/content/77/6/418
- Childhood immunisations and Covid-19: National trends showed reduced childhood immunisations during the pandemic; in Lambeth, high rates were maintained (88-89%) for the 6-in-1, meningitis B and rotavirus vaccines; pneumococcal vaccine fell by 9% but MMR rose by 8%; childhood flu vaccine also increased. There were no substantial ethnicity/socio-economic inequalities; Research lead: Rashmi D’Souza/Lizzie Cecil; presented at RCPCH national conference, June 2022.
- Long Term Opioid prescribing: This study found higher levels of long-term opioid prescribing in those with multimorbidity, older adults (aged over 75 years) and people with LTCs such as sickle cell disease, depression, rheumatoid arthritis, osteoarthritis and alcohol dependence. These findings can be used to target deprescribing initiatives at the most at-risk groups. Research lead: Mariam Molokhia, published in Br J Clin Pharmacol: https://doi.org/10.1111/bcp.15231
- Multimorbidity consultation rates: analysing data from 18 ethnicity categories, this study found that Caribbean patients with multimorbidity had the highest consultation rates. These high consultation rates appear to be driven by high rates of Chronic Pain, Depression, Asthma, Hypertension; Research lead: Siddesh Shetty (work in progress)
- Multimorbidity, Covid-19 and QOF indicator achievement: Overall, individuals from ethnic minority groups, the youngest (18-39), and most deprived were less likely to achieve QOF targets. Two specific QOF targets were poorly achieved, post-pandemic, in patients with multimorbidity: COPD008 (pulmonary rehab); DM019 (BP target in DM); Research Lead: Marina Soley-Bori; findings submitted to Br J Gen Pract (March 2023)